What's the story with Kaylas Cleft?
/
Anyone following my journey over the past year will know Kayla was born with a cleft palate (but not lip) Many people don’t quite understand what that means, and to be honest I struggled a bit at the beginning too! So I thought a blog would help :)
There are many different types of clefts and no two are the same. A baby can be born with a cleft lip, a cleft palate or both a cleft lip and cleft palate. Essentially what a cleft is, is a hole or gap in the area.
The following stats are taken from (http://www.cleft.ie/?page_id=25) The incidence of cleft lip and/or palate in Ireland is between 1 in 700 and 1 in 1,000 births. Incidence of cleft palate occuring alone is about 1 in 2000 births. More than 70% of babies with cleft lip also have cleft palate.
Parents who have a child born with a cleft, have a 5% chance of the next born also having a cleft (so a 1 in 20 chance). If a second child is born with a cleft, the likelihood increases further for any subsequent child.
The chances of a parent who was born with a cleft having a cleft baby is approximately 7 in 100. So Kayla will have roughly a 7% chance of having a baby with a cleft (of course if she chooses to be a parent but we would love lots of grandchildren!).
Types of Cleft Lip
Forme fruste unilateral cleft lip
A subtle cleft on one side of the upper lip, which may appear as a small indentation.Incomplete unilateral cleft lip
A cleft on one side of the upper lip, which does not extend into the nose.Complete unilateral cleft lip
A cleft on one side of the upper lip, which extends into the nose.Incomplete bilateral cleft lip
Clefts on both sides of the upper lip, not extending to the nose.Complete bilateral cleft lip
Clefts on both sides of the upper lip, extending into the nose.
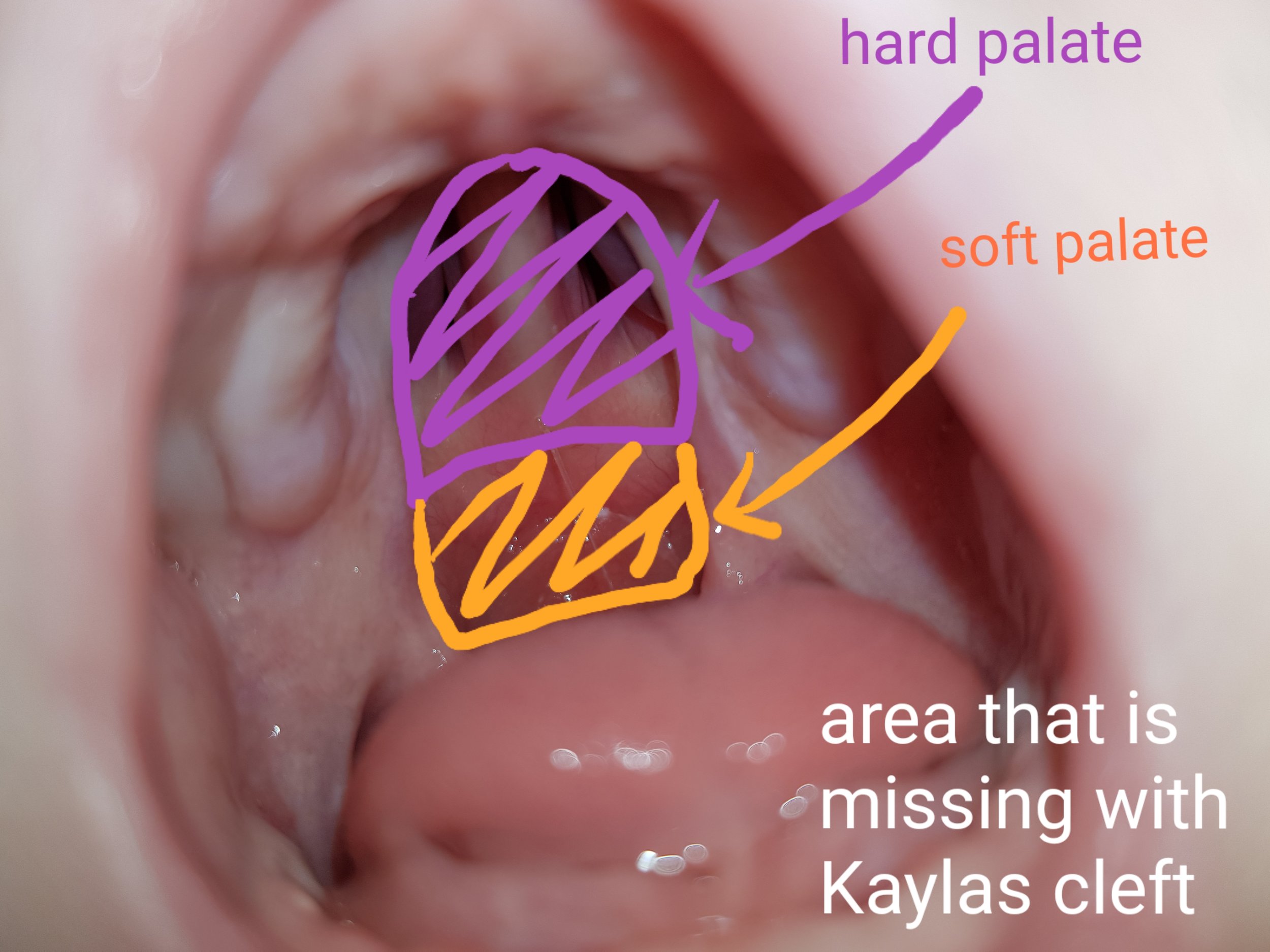
Types of Cleft Palate
Incomplete cleft palate
A cleft in the back of the mouth in the soft palate.Complete cleft palate
A cleft affecting the hard and soft parts of the palate. The mouth and nose cavities are exposed to each other.Submucous cleft palate
A cleft involving the hard and/or soft palate, covered by the mucous membrane lining the roof of the mouth. May be difficult to visualize.
Kayla is linked in with the cleft team in Temple Street. They have been amazing. Big shout out to Jane the cleft nurse specialist who takes families under her wing and walks the journey with them. She gives us so much time to ask any questions we may have and checks in regularly to see how Kayla is doing.
In Ireland, the cleft teams grade the palate or lip cleft from 0-3. 0 being very mild and 3 the most sever. Kayla has a grade 3 cleft palate. She has a complete cleft palate, but instead of just being a gap or a hole Kayla is missing all of her palate (hard and soft)
Kayla also has a condition called Pierre Robin sequence (or syndrome) PRS for short. This is a condition in which babies are born with a smaller than normal lower jaw, a tongue that is small and bunched which often falls back in the throat, and difficulty breathing. It is present at birth but not always detected in pregnancy ultrasounds. Most babies with PRS have a U shaped cleft palate like Kayla. Again the team will grade PRS 0-3 and Kayla scored a 0, as luckily she does not have many issues with her airways. Kayla does well once she is on her side or raised. Another positive is that nature gave her a helping hand with a tight posterior and anterior tongue tie to hold her tongue in place, so her tongue does not flop back to block her airways (who would have thought it? A helpful tongue tie!!)
Other common issues in babies/children with PRS are problems with their eyes (Stickler Syndrome), problems with their inner ears and dental issues. Kayla will be under different teams for each and so far they have been wonderful.
Kayla will have her first surgery to create a soft palate when she is around 9 months. This will hopefully help with her speech development. She will most likely be 3 years old before her palate is completely closed but for now it seems the only long term issue she will have is a speech delay – which she will catch up on by the time she is 10 years or so. So while her first few years of life will be hard, with surgeries and hospital appointments it is something that won’t hold her back and she can put behind her!
I hope this blog helps to explain things a little? Please feel free to ask questions :)
Again thank you to everyone for the love and support since Kayla was born xx
If you or someone you know has a baby with a cleft or PRS these are helpful resources:
Websites:
http://www.cleft.ie/
https://www.clapa.com/
www.cleftlipandpalatebreastfeeding.com
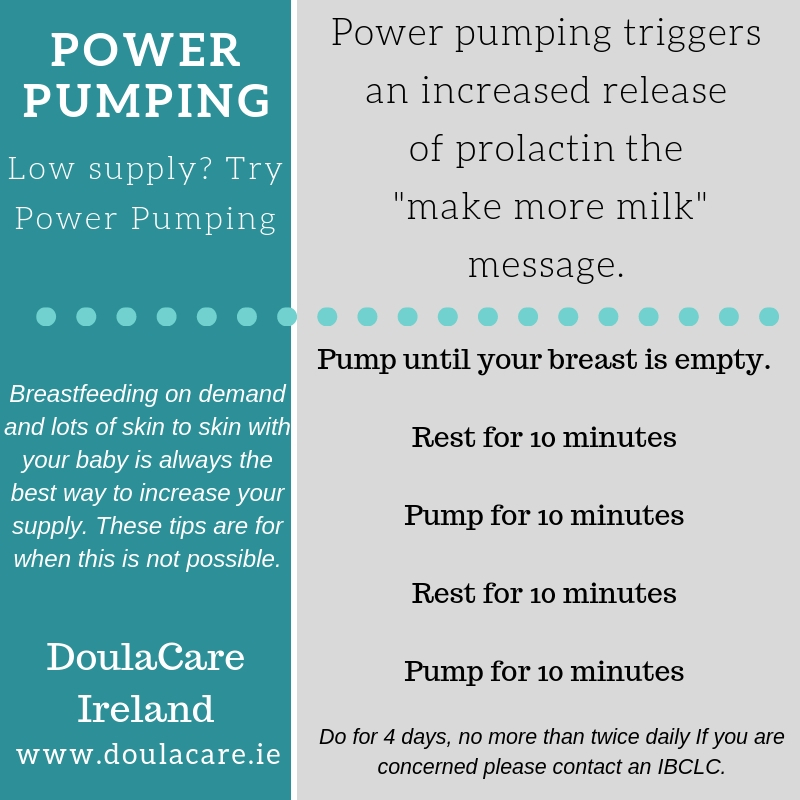
https://www.breastfeeding.ie/Resources/Publications/ The booklet I co created "Breastfeeding and Expressing for your preterm or sick baby" has lots of information on getting off to a good start, maintaining your milk supply, storing milk, skin to skin and more. It is available free to download or order. All Irish maternity units should have copies also.
The Australian Breastfeeding Association (ABA) has two booklets (both e-booklet -released during 2017 and hard copy) The cleft breastfeeding booklet: https://goo.gl/ZnoFqc has information about breastfeeding - and expressed breast milk feeding, lactation aids, type of feeding methods including - cup/spoon/supply lines/ bottles/teats. As well as some of the experiences surrounding feeding from families. The second booklet is all about expressing and storing breastmilk: https://goo.gl/ft7gDp.
Facebook pages:
cleft lip & palate association of ireland
Cleft Lip And Palate Association
Cleft Lip and Palate Breastfeeding Support Group